★
What is cervical cancer?
● Cervical
cancer is a type of cancer that begins in the cells lining the cervix, which is
the narrow end of the uterus that connects to the vagina. It is primarily
caused by the human papillomavirus (HPV), a sexually transmitted infection.
However, not all HPV infections lead to cervical cancer; certain strains of
HPV, particularly HPV 16 and 18, are considered high-risk and are more likely
to cause cervical cancer.
●
Cervical cancer typically progresses slowly, often
starting with precancerous changes in the cells of the cervix. These changes
can be detected through regular Pap smear screenings, allowing for early
treatment and prevention of cancer development. If left untreated, precancerous
changes can develop into invasive cervical cancer, which can spread to nearby
tissues and, eventually, to other parts of the body.
●
Common symptoms of cervical cancer may include abnormal
vaginal bleeding, such as bleeding between menstrual periods, after
intercourse, or after menopause, as well as pelvic pain and pain during
intercourse. However, in its early stages, cervical cancer may not cause any
symptoms, which is why regular screenings are crucial for early detection and
treatment.
●
Treatment options for cervical cancer depend on the stage
and extent of the cancer but may include surgery, radiation therapy,
chemotherapy, or a combination of these treatments. Vaccination against HPV is
also an effective preventive measure against cervical cancer, particularly when
administered before becoming sexually active.
★
What is the incidence in Gujarat, India,
world?
●
Globally, cervical
cancer remains a significant public health issue, particularly in low- and
middle-income countries where access to screening and preventive measures may
be limited. Efforts to increase awareness, improve screening programs, and
expand access to HPV vaccination can help reduce the incidence of cervical
cancer both in India and around the world.
★ What causes cervical
cancer?
● Cervical cancer is primarily caused by
persistent infection with certain types of human papillomavirus (HPV),
particularly HPV types 16 and 18. HPV is a common sexually transmitted
infection, and while most infections clear on their own, persistent infection
with high-risk HPV types can lead to the development of cervical cancer over
time.
●
Factors that
increase the risk of developing cervical cancer include:
●
HPV infection: Persistent infection with high-risk HPV
types, particularly HPV 16 and 18, is the primary cause of cervical cancer.
●
Weakened immune
system: A weakened immune system
due to conditions such as HIV/AIDS or immunosuppressive medications can
increase the risk of HPV infection progressing to cervical cancer.
●
Smoking: Smoking tobacco increases the risk of
cervical cancer. Chemicals in tobacco can damage cervical cells and make it
easier for HPV infections to persist and progress to cancer.
●
Early sexual
activity: Engaging in sexual activity
at an early age increases the risk of HPV infection, which in turn increases
the risk of cervical cancer.
●
Multiple sexual
partners: Having multiple sexual partners can increase the risk of HPV exposure
and infection.
●
Long-term use of
oral contraceptives: Some studies suggest
that long-term use of oral contraceptives may be associated with an increased
risk of cervical cancer, although the risk decreases after discontinuing their
use.
●
Poor socioeconomic
status: Limited access to
healthcare, including regular cervical cancer screening (Pap tests) and HPV
vaccination, can contribute to a higher risk of developing cervical cancer.
●
It's important to
note that while these factors increase the risk of developing cervical cancer,
not all individuals with these risk factors will develop the disease. Regular
screening with Pap tests and HPV testing, along with HPV vaccination, can help detect
precancerous changes early and prevent the development of cervical cancer.
★ What are the
symptoms?
In the early stages, cervical cancer may
not cause any symptoms, which is why regular screenings such as Pap tests are
crucial for early detection. As the cancer progresses, symptoms may develop.
Common symptoms of cervical cancer include:
●
Abnormal vaginal
bleeding:
○ Bleeding between menstrual periods
○
Bleeding after
sexual intercourse
○
Bleeding after
menopause
○ Heavier or longer menstrual periods than
usual
●
Unusual vaginal
discharge:
○
Watery, bloody, or
foul-smelling discharge from the vagina
●
Pelvic pain or pain
during intercourse:
○ Persistent pelvic pain not related to menstruation
or other conditions
○ Pain during sexual intercourse
(dyspareunia)
○
Pain or discomfort
during urination can occur if the cancer has spread to nearby tissues.
●
Changes in bowel
habits or urinary habits:
○ Constipation or changes in bowel habits
○
Blood in the stool
○
Difficulty urinating
or frequent urination
○
It's important to
note that these symptoms can also be caused by conditions other than cervical
cancer. However, if you experience any of these symptoms, particularly if they
are persistent or unusual for you, it's important to consult a healthcare
professional for evaluation and appropriate testing.
○ Early detection of cervical cancer
greatly improves the chances of successful treatment. Therefore, regular
cervical cancer screenings, such as Pap tests and HPV testing, are recommended
for all individuals with a cervix, starting at age 21 or as recommended by a
healthcare provider.
★
What are the risk factors for cervical
cancer?
● Several factors can increase the risk of
developing cervical cancer. These include:
●
Human Papillomavirus
(HPV) infection: Persistent
infection with high-risk types of HPV, particularly HPV 16 and HPV 18, is the
most significant risk factor for cervical cancer.
●
Sexual activity: Early initiation of sexual activity and
having multiple sexual partners increase the risk of HPV infection, which in
turn increases the risk of cervical cancer.
●
Weakened immune
system: Conditions or medications
that weaken the immune system, such as HIV/AIDS or immunosuppressive drugs, can
make individuals more susceptible to HPV infection and increase the risk of
cervical cancer.
●
Smoking: Tobacco use, including smoking
cigarettes or exposure to second hand smoke, is associated with an increased
risk of cervical cancer. Smoking may weaken the immune system's ability to
fight HPV infection and also damage cervical cells.
●
Family history: Having a family history of cervical
cancer or precancerous cervical lesions may increase the risk of developing the
disease. Genetic factors may play a role in some cases.
●
Long-term use of
oral contraceptives: Some studies
suggest that long-term use of oral contraceptives (birth control pills) may be
associated with a slightly increased risk of cervical cancer. The risk may
decrease after discontinuation of oral contraceptives.
●
Socioeconomic
factors: Limited access to
healthcare, including cervical cancer screening (Pap tests) and HPV
vaccination, as well as factors such as poverty and low education level, may
increase the risk of cervical cancer.
●
Dietary factors: A diet low in fruits and vegetables may
be associated with an increased risk of cervical cancer. Adequate intake of
certain nutrients, such as folate, may play a protective role against the
development of cervical cancer.
●
Sexually transmitted
infections (STIs): Some sexually
transmitted infections, such as chlamydia, may increase the risk of cervical
cancer, although the association is not as strong as with HPV infection.
●
It's important to
note that having one or more of these risk factors does not necessarily mean
that someone will develop cervical cancer. Likewise, not having any of these
risk factors does not guarantee protection against the disease. Regular
cervical cancer screenings and preventive measures, such as HPV vaccination,
are important for early detection and prevention of cervical cancer.
★
Can I lower my risk of getting cervical
cancer?
● Yes, there are several steps you can take
to lower your risk of developing cervical cancer:
●
Get vaccinated
against HPV: The HPV vaccine is highly
effective in preventing infection with the most common high-risk types of HPV,
including types 16 and 18, which are responsible for the majority of cervical
cancer cases. The vaccine is recommended for both boys and girls starting at
age 9 to 12, although it can be given up to age 26 for females and up to age 21
for males who have not previously been vaccinated.
●
Practice safe sex: Using condoms consistently and
correctly during sexual activity can reduce the risk of HPV infection, although
they do not provide complete protection since HPV can infect areas not covered
by the condom.
●
Get regular cervical
cancer screenings: Regular
screenings, such as Pap tests (also called Pap smears) and HPV tests, can
detect precancerous changes in the cervix early, allowing for timely treatment
and prevention of cervical cancer. The recommended screening guidelines may
vary depending on age, risk factors, and previous screening results, so it's
essential to discuss screening options with your healthcare provider.
●
Quit smoking: Smoking tobacco is associated with an
increased risk of cervical cancer, as it can weaken the immune system and
damage cervical cells. Quitting smoking can reduce your risk of developing
cervical cancer and provide numerous other health benefits.
●
Limit your number of
sexual partners: Having multiple
sexual partners increases the risk of HPV infection, which in turn increases
the risk of cervical cancer. Limiting the number of sexual partners and
practicing monogamy can help reduce your risk.
●
Maintain a healthy
diet: Eating a balanced diet
rich in fruits, vegetables, and whole grains may help reduce the risk of
cervical cancer. Adequate intake of certain nutrients, such as folate, may play
a protective role against the development of cervical cancer.
●
Practice good
hygiene: Keeping the genital area
clean and practicing good hygiene habits can help reduce the risk of developing
cervical infections, including HPV.
●
By incorporating
these preventive measures into your lifestyle, you can significantly lower your
risk of developing cervical cancer and promote overall health and well-being.
Additionally, staying informed about cervical cancer and discussing any concerns
with your healthcare provider can help ensure appropriate screening and
preventive care.
★ How can I
preserve my quality of life during treatment?
● Maintaining a good quality of life during
cervical cancer treatment involves addressing physical, emotional, and
practical aspects of care. Here are some strategies to help preserve your
quality of life during treatment:
●
Stay informed: Educate yourself about your treatment
options, potential side effects, and ways to manage them. Ask your healthcare
team questions and seek clarification whenever necessary. Understanding what to
expect can help alleviate anxiety and empower you to make informed decisions
about your care.
●
Build a support
network: Surround yourself with
supportive friends, family members, and healthcare professionals who can offer
emotional support and practical assistance. Joining support groups or seeking counselling
can also provide valuable support and guidance throughout your treatment
journey.
●
Maintain a healthy
lifestyle: Eat a balanced diet rich in
fruits, vegetables, whole grains, and lean proteins to support your overall
health and well-being. Stay hydrated and try to engage in light physical
activity, such as walking or gentle stretching exercises, as tolerated. Avoid
smoking and limit alcohol consumption to promote healing and reduce the risk of
complications.
●
Manage treatment
side effects: Work closely with your
healthcare team to manage any side effects of treatment, such as nausea,
fatigue, pain, or changes in appetite. They can recommend medications,
lifestyle modifications, or complementary therapies to help alleviate
discomfort and improve your quality of life.
●
Prioritize
self-care: Make time for activities
that bring you joy and relaxation, whether it's reading, listening to music,
practicing meditation or mindfulness, or spending time in nature. Engaging in
self-care activities can help reduce stress and improve your overall well-being
during treatment.
●
Communicate openly: Be honest with your healthcare team about
your concerns, preferences, and treatment goals. Open communication can help
ensure that your needs are addressed effectively and that you receive
personalized care tailored to your individual circumstances.
●
Plan for practical
needs: Address practical
considerations, such as transportation to and from medical appointments,
childcare, household chores, and financial concerns. Enlist the help of
friends, family members, or community resources to assist with tasks as needed,
allowing you to focus on your recovery and well-being.
●
Seek emotional
support: Acknowledge and express
your feelings openly, whether it's fear, sadness, anger, or uncertainty. Talk
to a trusted friend, family member, counsellor, or support group about your
emotions and concerns. It's okay to ask for help and to seek professional
support when needed.
●
Stay hopeful: Maintain a positive outlook and focus on
the progress you're making, no matter how small. Celebrate victories, whether
it's completing a round of treatment, achieving a personal milestone, or simply
getting through a challenging day. Finding meaning and purpose in your journey
can help sustain your resilience and optimism.
●
Remember that
everyone's experience with cervical cancer treatment is unique, and it's
important to prioritize self-care and well-being throughout the process. By
taking proactive steps to address physical, emotional, and practical needs, you
can help preserve your quality of life and enhance your overall sense of
resilience and well-being during treatment.
★ How long
does it take for cervical cancer to develop?
● The development of cervical cancer
typically occurs over a period of several years, often starting with
precancerous changes in the cells of the cervix. These precancerous changes,
known as cervical dysplasia or cervical intraepithelial neoplasia (CIN), can
progress to invasive cervical cancer if left untreated.
●
The timeline for the
development of cervical cancer can vary widely from person to person and
depends on various factors, including:
●
HPV infection: Persistent infection with high-risk types
of human papillomavirus (HPV), particularly HPV 16 and HPV 18, is the primary
risk factor for cervical cancer. The duration and persistence of HPV infection
can influence the progression to cervical cancer.
●
Immune response: The body's immune response to HPV
infection can play a role in determining whether precancerous changes progress
to invasive cancer. Factors that weaken the immune system, such as HIV/AIDS or
immunosuppressive medications, may increase the risk of progression.
●
Individual factors: Other individual factors, such as
genetics, lifestyle choices (such as smoking), and coexisting medical
conditions, can also influence the development and progression of cervical
cancer.
●
In general, it can
take several years for precancerous changes to develop into invasive cervical
cancer. However, the progression from precancerous changes to cancer can vary
in speed, and in some cases, cervical cancer may develop more rapidly.
● Regular cervical cancer screening, such
as Pap tests (Pap smears) and HPV testing, is essential for early detection and
prevention of cervical cancer. Screening can detect precancerous changes in the
cervix before they progress to cancer, allowing for timely intervention and
treatment. Additionally, vaccination against HPV can help prevent infection
with high-risk HPV types and reduce the risk of cervical cancer in the long
term.
★
What are the most common surgical procedures?
● Several surgical procedures may be used
in the treatment of cervical cancer, depending on the stage of the cancer and
individual patient factors. Some of the most common surgical procedures for
cervical cancer include:
●
Conization (or cone
biopsy): This procedure involves
removing a cone-shaped piece of tissue from the cervix. Conization is often
used to diagnose and treat early-stage cervical cancer or precancerous lesions.
It can be performed using a scalpel (cold knife conization), laser, or loop
electrosurgical excision procedure (LEEP).
●
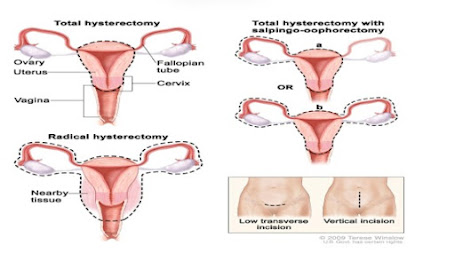
Radical
hysterectomy: In a radical hysterectomy,
the surgeon removes the uterus, cervix, upper part of the vagina, and
surrounding tissues, including lymph nodes. This procedure is typically
recommended for early-stage cervical cancer that has not spread beyond the
cervix.
●
Pelvic
lymphadenectomy: During a pelvic
lymphadenectomy, the surgeon removes lymph nodes from the pelvic area to
determine if cancer has spread beyond the cervix. This procedure may be
performed in conjunction with a radical hysterectomy or as a separate
procedure.
●
Trachelectomy: A trachelectomy is a fertility-preserving
surgical procedure that involves removing the cervix while preserving the body
of the uterus. This procedure may be an option for select women with
early-stage cervical cancer who wish to preserve their fertility.
●
Pelvic exenteration:
In cases of advanced or recurrent
cervical cancer, pelvic exenteration may be performed. This extensive surgery
involves removing the uterus, cervix, vagina, surrounding tissues, and nearby
organs such as the bladder, rectum, or part of the colon. It is typically
reserved for cases where other treatments have been unsuccessful.
●
Minimally invasive
surgery: Minimally invasive
surgical techniques, such as laparoscopic or robotic-assisted surgery, may be
used for certain cervical cancer surgeries, including radical hysterectomy and
pelvic lymphadenectomy. These techniques involve making small incisions and using
specialized instruments and cameras to perform the surgery with less trauma and
faster recovery compared to traditional open surgery.
●
The choice of
surgical procedure depends on factors such as the stage and location of the
cancer, the patient's overall health and preferences, and the expertise of the
surgical team. Your healthcare provider will discuss the available options with
you and help determine the most appropriate treatment plan for your individual
situation.
★ What is a
pap test?
● A Pap test, also known as a Pap smear, is a
screening test used to detect abnormal changes in the cells of the cervix,
which is the lower part of the uterus that connects to the vagina. The Pap test
is primarily used to screen for cervical cancer and precancerous conditions.
●
During a
Pap test, a healthcare provider uses a small brush or spatula to collect cells
from the surface of the cervix. The collected cells are then placed on a glass
slide or in a liquid solution and sent to a laboratory for examination under a
microscope. In the laboratory, trained professionals (cytotechnologists or
pathologists) examine the cells for any abnormalities, such as changes in size,
shape, or appearance.
●
The Pap
test can detect early signs of cervical cancer, as well as precancerous changes
called cervical dysplasia or cervical intraepithelial neoplasia (CIN).
Detecting these changes early allows for timely intervention and treatment to
prevent the development of cervical cancer.
●
It's
important to note that the Pap test does not diagnose cervical cancer itself;
instead, it detects abnormal changes in the cervical cells that may indicate an
increased risk of developing cervical cancer. If abnormal cells are found on a
Pap test, further evaluation, such as additional testing or a colposcopy
(examination of the cervix with a magnifying instrument), may be recommended to
determine the appropriate next steps.
● Regular Pap testing is recommended for most women
starting at age 21 and continuing at regular intervals as recommended by their
healthcare provider. The frequency of Pap testing may vary depending on factors
such as age, previous Pap test results, and personal medical history.
Additionally, the Pap test may be combined with HPV testing for certain age
groups or risk factors to improve cervical cancer screening accuracy.
★
What is the government's help in
preventing this disease?
● Governments play a crucial role in
preventing cervical cancer and promoting public health through various
initiatives and policies. Some ways in which governments help prevent cervical
cancer include:
●
HPV vaccination
programs: Governments often implement
vaccination programs to make the HPV vaccine available to eligible populations.
These programs may target adolescents and young adults, aiming to vaccinate
individuals before they become sexually active and are at risk of HPV infection.
Governments may provide the HPV vaccine free of charge or at a reduced cost
through schools, healthcare facilities, or community vaccination clinics.
●
Cervical cancer
screening programs: Governments may
establish cervical cancer screening programs to ensure that eligible
individuals have access to regular Pap tests or HPV testing. These programs may
include guidelines for screening intervals, outreach efforts to underserved
populations, and strategies to increase screening rates. Governments may also
provide funding for screening services and follow-up care for individuals with
abnormal test results.
●
Public awareness
campaigns: Governments may launch
public awareness campaigns to educate the public about cervical cancer risk
factors, prevention strategies, and the importance of vaccination and
screening. These campaigns may utilize various channels, such as television,
radio, social media, and community outreach events, to disseminate information
and raise awareness.
●
Healthcare
infrastructure and resources: Governments invest
in healthcare infrastructure and resources to ensure that individuals have
access to high-quality preventive care, diagnosis, and treatment services for
cervical cancer. This may include funding for healthcare facilities, equipment,
trained healthcare professionals, and research initiatives to advance knowledge
and innovation in cervical cancer prevention and treatment.
●
Policy development
and advocacy: Governments develop
policies and guidelines to support cervical cancer prevention efforts, such as
vaccination requirements for school entry, reimbursement policies for HPV
vaccines and screening tests, and regulations to ensure the safety and efficacy
of vaccines and screening tests. Governments may also advocate for global
initiatives to address cervical cancer as a public health priority and
collaborate with international organizations, such as the World Health
Organization (WHO), to support global efforts to prevent cervical cancer.
●
Overall, government
involvement is essential in implementing comprehensive cervical cancer
prevention strategies, reducing disparities in access to care, and ultimately,
saving lives through early detection and treatment. By prioritizing cervical
cancer prevention and investing in evidence-based interventions, governments
can make significant strides in reducing the burden of cervical cancer on
public health